
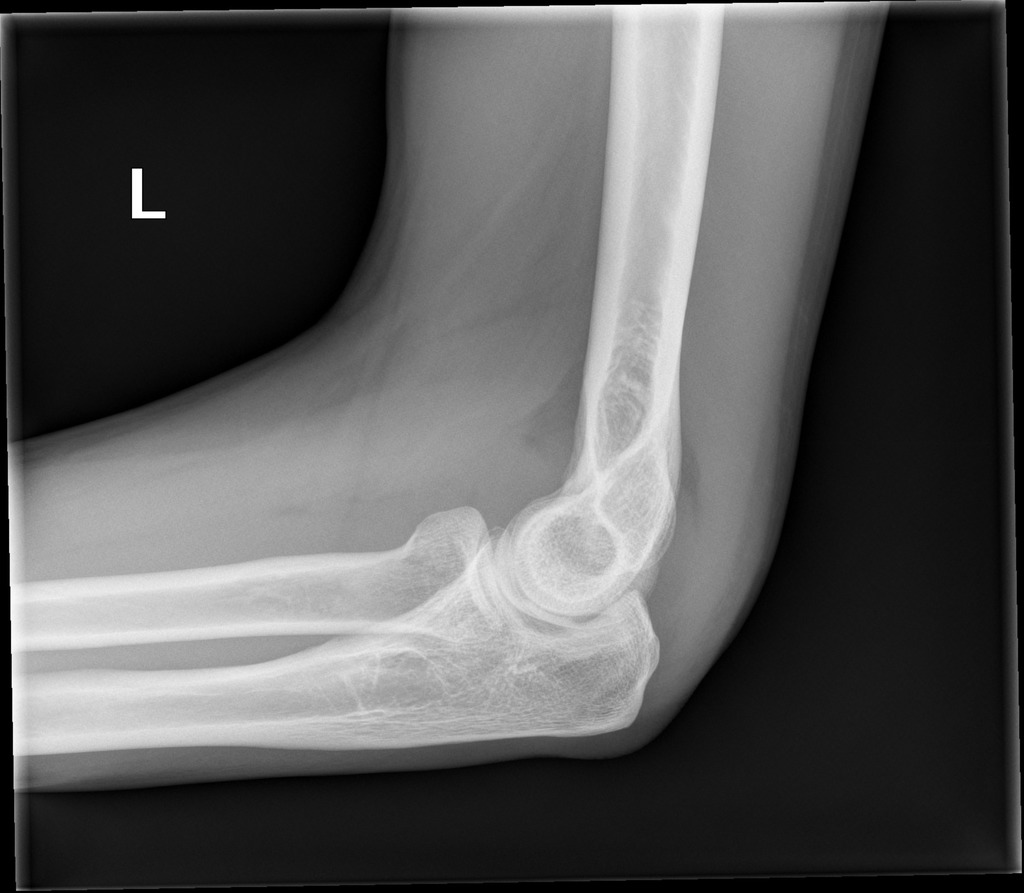
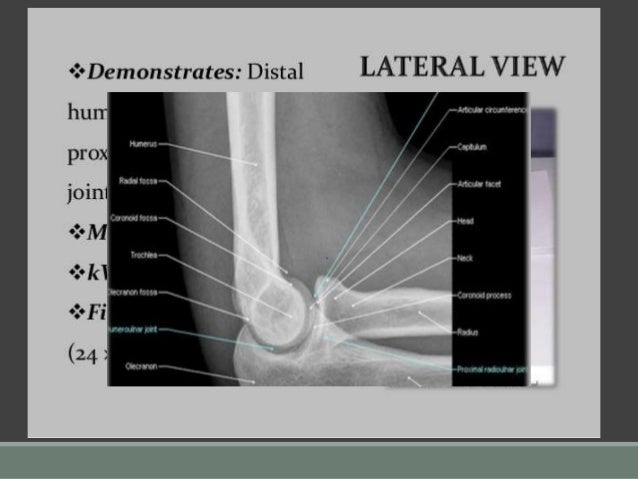
Patients should be kept nil orally until a decision about surgery is made. Do I need to refer to orthopaedics now?ĭue to the potential for poor outcomes, all lateral condyle fractures require prompt orthopaedic consultation. No reduction is required.Ģ mm gap and/or angulation of the lateral condyle) will need to go to theatre either for closed reduction and percutaneous pinning or open reduction. Undisplaced fractures can be immobilised in an above-elbow backslab with the elbow flexed to 90 degrees. When is reduction (non-operative and operative) required? Notice that the majority of the soft tissue is located laterally.ħ. It shows a displaced fracture fragment (>2 mm). The AP in this instance provides the most useful information. Minimally displaced lateral condyle fracture (2 mmįigure 3: AP and lateral view of a displaced lateral condyle fracture (Milch type I) in a four year old boy. Oblique views may be useful in undisplaced lateral condyle fractures. The presence of anterior and posterior fat pad signs may be the only clue. An undisplaced lateral condyle fracture may be difficult to see on plain x-ray. What do they look like on x-ray? Undisplaced lateral condyle fractureįigure 1: Three year old girl with an undisplaced fracture of the lateral condyle. This allows subtle fracture lines to be more visible on x-ray.Ħ. These fractures do not require splinting prior to imaging as there is usually less pain and swelling. If a lateral condyle fracture is suspected or minimally displaced on x-rays, then oblique views are often useful. If there is clinical suspicion of injury in the forearm or wrist then separate films of these areas should be ordered. What radiological investigations should be ordered?Īnteroposterior (AP) and lateral x-rays of the elbow should be obtained without splinting. Lateral condyle fractures can frequently look benign with minimal swelling and minimal deformity, which can lead to delays in presentation and recognition of the fracture.ĥ. The child will present with pain, limited elbow range of motion (ROM) and swelling at the lateral aspect of the elbow. Angular and rotational forces are thought to contribute. They usually occur as a result of indirect forces being applied to the elbow following a fall on an outstretched hand. They account for 12-20% of elbow fractures in children. Lateral condyle fractures of the elbow are the second most common paediatric elbow fracture after supracondylar fractures.

How common are they and how do they occur? The fracture line runs medial to the capitellar ossification centreĮquivalent to a Salter-Harris type II fractureģ. The fracture line goes through the capitellar ossification centreĮquivalent to a Salter-Harris type IV fracture Table 1: Milch classification of lateral condyle fractures. The Milch classification system (Table1) classifies the fracture according to the location of the fracture line in relation to the capitellar ossification centre. Lateral condyle fractures involve a fracture line entering into the elbow joint. Follow-up in fracture clinic should occur within 7 days with x-ray.Ģ mm gap and/or angulation of the lateral condyle) will need to go to theatre either for closed reduction and percutaneous pinning or open reduction. Undisplaced fractures can be immobilised in an above-elbow backslab with the elbow flexed to 90 degrees and supported in a sling. Prompt recognition and treatment are essential to avoid complications and prevent functional impairment. What are the potential complications associated with this injury?ĭue to the potential poor outcomes, all lateral condyle fractures require prompt orthopaedic consultation.What is the usual ED management for this fracture?.Do I need to refer to orthopaedics now?.When is reduction (non-operative and operative) required?.

What radiological investigations should be ordered?.How common are they and how do they occur?.
Lateral condyle fracture of the humerus - Fracture clinics


 0 kommentar(er)
0 kommentar(er)
